Book Online
Previous
Next
Just choose the appointment type and time that work best for you, and you're on your way to clear, comfortable vision!

Keratoconus is a progressive, deforming disease of the cornea with a strong genetic component. However, new advances in technology have allowed us to slow, stop, and sometimes even slightly reverse this sight-threatening condition.
Just choose the appointment type and time that work best for you, and you're on your way to clear, comfortable vision!
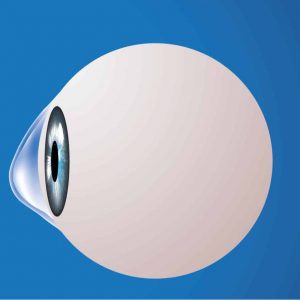
Keratoconus is a deformation of the cornea, which is the clear, front-most portion of your eye. The shape of your cornea determines whether you are near-sighted, far-sighted, or have astigmatism and is responsible for 2/3 of the focusing power of the eye. Normally, the cornea has a spherical shape. In keratoconus, the internal infrastructure of the cornea breaks down, causing the cornea to take on a conic shape so that it ends up looking like an ice-cream cone. As the shape of the cornea starts to distort, so does the vision. Keratoconus usually affects one eye more than the other, stabilizes in the mid thirties, and typically does not result in blindness.
Keratoconus occurs when the cornea does not have the proper enzyme and anti-oxidant mixture to protect the internal scaffolding that gives the cornea it’s shape. The scaffolding is made of collagen fibrils that are constantly bombarded by oxidative free radicals as part of the cornea’s metabolic process. Normally, the corneal enzymes and anti-oxidants protect the collagen fibrils, but without them, the fibrils become damaged, weaken, and the cornea deforms, resulting in a bulged shape.
The main risk factors for keratoconus are:
Genetics: Patients have a higher risk of developing keratoconus if they have the following genetic conditions:
Chronic eye inflammation: Chronic inflammation, which can produce corneal damage resulting in keratoconus.
Eye rubbing: Chronic/vigorous eye rubbing is associated with developing/progressing keratoconus.
Age: Keratoconus is often discovered in the teenage years and continues to progress into the mid-thirties.
Keratoconus occurs in approximately one in 2,000 individuals.
Frequent prescription changes
Sudden worsening or clouding of vision
Glare and halos around lights
Difficulty seeing at night
Eye irritation or headaches associated with eye pain
Increased sensitivity to bright light
Treatment for keratoconus depends upon its severity.
Early Stages: In the early stages, glasses and soft contact lenses can be used to treat the blurred vision.
Intermediate Stages
Advanced Stages
| Monday - Thursday |
|
||
| Friday |
|
||
| Saturday | Closed | ||
| Sunday | Closed |
